My sophomore English teacher knew before I did. The exact details of the conversation are lost to me, but I’m sure we were discussing why a paper of mine was late. When I told him that my need to be multitasking at all times made it seem like I had ADHD or something, I thought it was a joke. I’d never been tested for attention deficit-hyperactivity disorder, and I had diagnosed myself as smart but lazy, squandering the potential reflected in my test scores. But my teacher did something I didn’t expect, which most likely altered the course of my life: He took me seriously.
He saw what I couldn’t at the time: My struggles with executive function fit with an ADHD diagnosis. Though I wasn’t formally diagnosed at the time, he and his co-teacher, who taught history, would give me extra time to turn in papers both that year and when I had them again my senior year. They believed me when I said they would get done eventually and graded them as though they were on time. It was the best they could do, seeing my struggles and not wanting to fault me for something they recognized as outside my control.
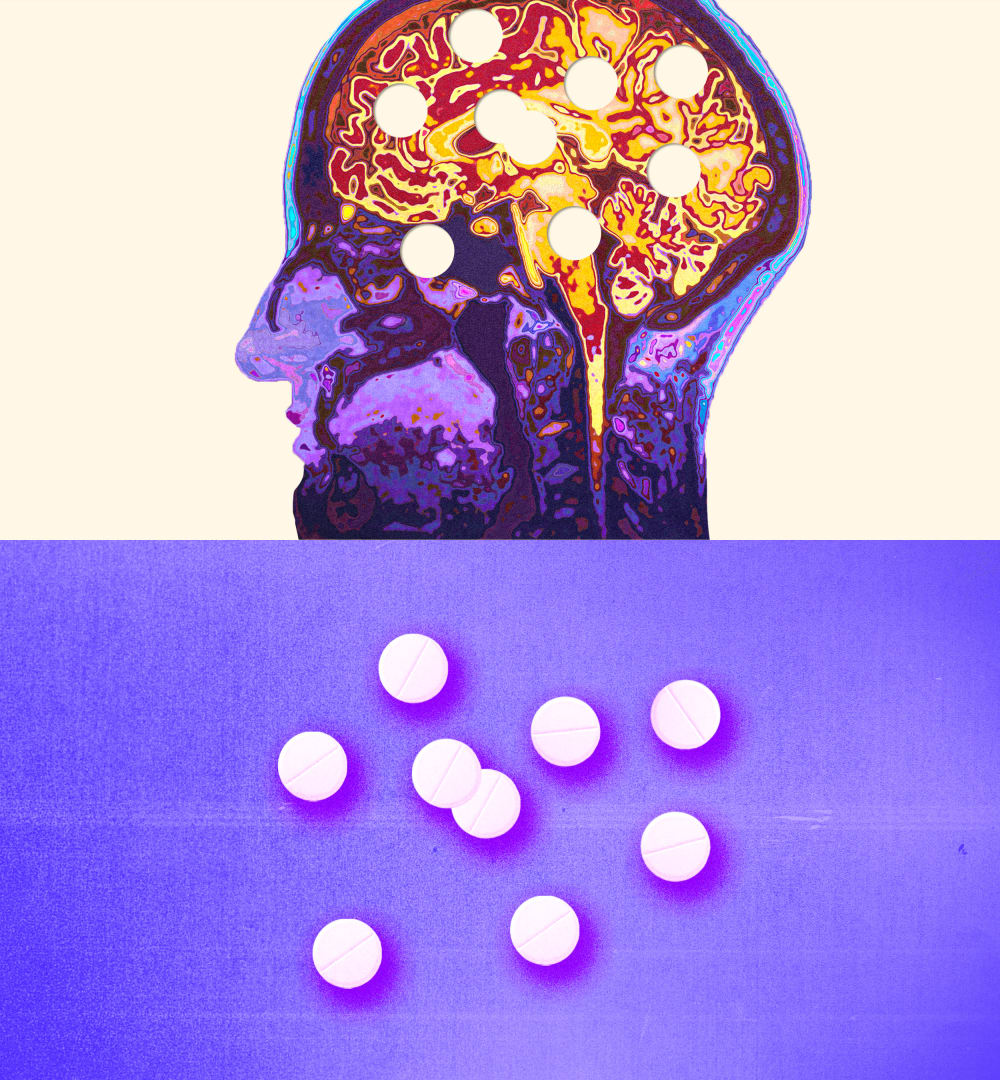
For over half a year now, patients around the country have struggled to fill their Adderall prescriptions, threatening to topple the structures ADHD patients have built up to support themselves.
It has been four years since I received my ADHD diagnosis from a psychiatrist. Only when I announced it on Facebook did my former teacher relay his side of that story to me. In the years since, I’ve taken Adderall, or its generic version, almost every day at varying dosages to help me function in a society in which any lack of productivity is seen as a moral failing. Before then, I’d been decent enough at most of the jobs I’d held, terrible at others. After I began treatment, I could actually remember what I was in the middle of doing as I was doing it. I didn’t feel the need to get up to wander the office every few minutes. I could motivate myself to start projects even when there were more promising distractions. It was a revelation.
Even during the depths of the pandemic, I was fortunate to retain access to my prescription. It’s only lately that things are no longer quite so certain. For over half a year now, patients around the country have struggled to fill their Adderall prescriptions, threatening to topple the structures ADHD patients have built up to support themselves. The shortage, which has still never been fully explained, has revealed just how fragile the support system is for the millions of Americans like me — and how little policymakers seem to care about strengthening it.

My story isn’t unique; if anything, it has become more and more common over the last half-decade as diagnosis rates for ADHD in adults have soared. The “why” of that increase is complex and still not fully understood. Doctors and medical experts once considered ADHD a childhood disease, something that someone grew out of as the hyperactivity diminished with age. More recent research has emphasized the struggles with focus and organization, leading to rising diagnoses in adults and even seniors.
There’s no official nationwide tracking system for ADHD, which one 2021 study estimates as affecting “approximately 6% in children and 3% in adults” worldwide. Among the data we do have, a 2019 study found a 43% increase in the rate of adults’ being newly diagnosed with ADHD from 2007 to 2016. (Those numbers have most likely increased further in the aftermath of the Covid pandemic, when the rate of stimulant prescriptions jumped significantly.)
In the early 2000s, the prevailing image of an ADHD child was a white suburbanite preteen running laps around a classroom without his Ritalin.
Part of that surge is most likely the result of missed diagnoses when patients were younger. In the early 2000s, the prevailing image of an ADHD child was a white suburbanite preteen running laps around a classroom without his Ritalin. Young women and people of color were overlooked. The new focus on the inattentive side of the disorder, which presents more frequently in women, may also help explain the sharp uptick in diagnosis rates, as those symptoms tend to linger longer than the hyperactive ones. One of the lead authors of the 2019 study, which looked at patients treated in the Kaiser Permanente Northern California medical system, told CNN he was “encouraged by the fact that the recognition of ADHD in adults is increasing and disparities decreasing, though alarmed by the substantial work still needed to remove such disparities.”
At the same time, it’s impossible not to wonder how much of the boost comes from the spate of self-diagnosis via TikTok and memes that have become ubiquitous. Last year, a Canadian study found that about half of the most popular ADHD-related videos it studied on TikTok were misleading. The rise of telehealth during the early pandemic also led to a surge in potentially predatory ads from companies that offered fast and easy diagnoses for ADHD. The Federal Trade Commission and the Justice Department have launched investigations into the practice and whether these businesses have been overprescribing controlled substances.
Whatever the reason, the surge in demand has been met in the last several months with a depletion in the supply of ADHD medications. Anecdotally, I had been hearing about the struggles my friends have had for months. I managed to avoid it for the most part, being on a high dose of the extended-release formula. But in February, my local pharmacy told me its order was backlogged. It would remain so for the next month, forcing me to dip into a supply of older low-dose instant release pills that I’d saved for just such an emergency.
I could tell that their effectiveness had dulled slightly by the time I reached near the end of my supply. I was fortunate enough that my pharmacy had a supply of a slightly lower dose of the extended-release formula when my next appointment with my psychiatrist came around late last month. Thousands of people around the country weren’t so lucky and were left without any backstop once their prescriptions were fully depleted.
Much as with the increase in diagnoses, the causes of the shortages are under dispute. Teva, the largest manufacture of Adderall pills, revealed in July that it expected delays for the next several months. The company has blamed the resulting backlog on the Drug Enforcement Administration’s strict quotas for how much amphetamine is produced and doled out to Adderall manufacturers. That quota is based in part on the Food and Drug Administration’s estimates for how much Adderall will be needed each year.
But a DEA spokesperson told Bloomberg News in February that the companies had more than enough amphetamine on hand last year, with companies that needed more able to ask for increases in their allocations. The spokesperson said that in “2020, 2021 and 2022, the agency didn’t allot the entirety of the quota,” but neither the DEA nor manufacturers would say which companies — if any — actually asked for more amphetamine for their factories. Months into the shortage, the FDA’s database still lists many dosages of Adderall and its generic versions as unavailable, available only to existing contracted businesses, on back order or with “limited supply available, recovery TBD.”